Alzheimer’s research has gained immense importance as scientists strive to understand the underlying mechanisms of this debilitating disease. At the forefront of this battle is neuroscientist Beth Stevens, who has dramatically advanced our knowledge of microglial cells—an essential component of the brain’s immune system. Her groundbreaking work reveals how these cells can contribute to neurodegenerative diseases by improperly pruning synapses, which may ultimately lead to Alzheimer’s. By identifying novel biomarkers for Alzheimer’s, Stevens and her team are paving the way for innovative treatments that could benefit millions affected by this condition. As research evolves, the insights gained from these studies promise to usher in a new era of hope for countless individuals and their families.
The quest to combat forms of dementia, particularly Alzheimer’s disease, showcases the ever-evolving landscape of scientific exploration into cognitive decline. Investigators like Beth Stevens are uncovering the critical roles of glial cells, specifically microglia, which are pivotal in maintaining brain health and cleaning up cellular debris. These immune cells not only protect the brain but also play a crucial part in synaptic connections, underlining their significance in understanding neurodegenerative disorders. With advances in identifying key biological markers associated with Alzheimer’s, the research could lead to breakthroughs in treatment and prevention strategies. The implications of such findings extend beyond Alzheimer’s, raising hopes for interventions in a range of related neurodegenerative conditions.
Understanding Microglial Cells: The Brain’s Immune System
Microglial cells play a crucial role in maintaining the health and functionality of the brain. Often referred to as the brain’s immune system, these cells are responsible for detecting and responding to injury and disease. They constantly survey the neural environment, removing dead or damaged cells and pruning synapses to optimize communication among neurons. However, an imbalance in this pruning process can contribute to the pathogenesis of neurodegenerative diseases such as Alzheimer’s. By understanding how microglia operate, researchers can glean insights into the underlying mechanisms that lead to these devastating conditions.
The research spearheaded by Beth Stevens at Boston Children’s Hospital has been pivotal in expanding our knowledge of microglial behavior. Her lab’s findings suggest that abnormal microglial activity not only exacerbates Alzheimer’s disease but may also play a role in other conditions such as Huntington’s disease. The implications of these discoveries extend far beyond academic curiosity; they open doors to developing new therapeutic strategies and biomarkers for Alzheimer’s and similar neurodegenerative diseases, potentially improving outcomes for millions affected by these disorders.
Beth Stevens and the Fight Against Alzheimer’s Disease
Beth Stevens has emerged as a leading figure in the quest to understand and combat Alzheimer’s disease. By focusing on the role of microglial cells, her work has transformed the understanding of how these cells can both protect and harm the brain. Stevens emphasizes the importance of foundational research, noting how initial studies in the visual systems of mice laid the groundwork for significant advancements in Alzheimer’s science. This approach underscores the value of curiosity-driven research, which often reveals unexpected connections to human health.
The insights gained from Stevens’ research can lead to the identification of new biomarkers for Alzheimer’s, allowing for earlier detection and intervention. With approximately 7 million Americans facing this incurable disease, Stevens’ work not only represents scientific progress but also offers hope for improved treatment options. By unraveling the complexities of the brain’s immune response, her lab is forging a path toward innovative therapies that could change the landscape of Alzheimer’s care for future generations.
Understanding the intricate mechanics of microglial activity is crucial, as it could ultimately influence drug development and treatment protocols. By targeting the pathways through which microglia operate, researchers could mitigate their harmful effects on neuronal health, thus slowing or even reversing the progression of Alzheimer’s. Stevens’ work exemplifies how persistent inquiry into basic science can yield transformative applications in neurology and beyond.
The Role of Biomarkers in Alzheimer’s Research
Biomarkers for Alzheimer’s disease are critical for accurate diagnosis and the development of effective treatment strategies. As research progresses, identifying specific biological indicators tied to microglial activity is becoming increasingly important. These biomarkers could provide insights into the disease’s progression, enabling clinicians to tailor more personalized treatment plans for patients. Incorporating such biomarkers in clinical practice could significantly enhance the management of Alzheimer’s, making early intervention more feasible.
The Stevens Lab’s work on microglial function has the potential to revolutionize the way we approach Alzheimer’s research and patient care. By pinpointing the specific roles of microglial cells in disease pathology, researchers can move toward creating targeted therapies that address the root causes rather than just the symptoms of Alzheimer’s. The ongoing exploration of these biomarkers, alongside novel therapeutic pathways, signifies a hopeful direction in the fight against neurodegenerative diseases, ultimately benefiting the millions affected by Alzheimer’s.
Neurodegenerative Diseases: Challenges and Innovations
Neurodegenerative diseases, including Alzheimer’s, pose significant challenges for modern medicine. Research has shown that the mechanisms underlying these diseases are often complex, involving degeneration of neurons and disruptions in cellular communication. Microglial cells, as pivotal players in the brain’s immune system, are increasingly recognized for their dual role in both protecting and damaging neural tissues. Understanding these mechanisms is essential for developing innovative therapies to combat neurodegenerative diseases.
Innovative approaches to studying neurodegenerative diseases focus on the interaction between microglial activity and neural health. Beth Stevens’ research is a prime example, as it highlights the vital need for continued investment in basic science to uncover these intricate relationships. The insights gained from studying diseases like Alzheimer’s not only enhance our understanding of these conditions but also pave the way for groundbreaking advancements in treatment modalities that could ultimately improve patient outcomes across the board.
The Importance of Federal Funding in Alzheimer’s Research
Federal funding plays a crucial role in advancing Alzheimer’s research, providing the necessary resources for groundbreaking studies like those conducted by Beth Stevens. Support from institutions such as the National Institutes of Health enables researchers to pursue innovative ideas and long-term projects that may not receive funding through traditional channels. Such investments are essential for cultivating scientific inquiry that can eventually translate into significant medical breakthroughs.
The commitment of federal agencies to Alzheimer’s research has fostered an environment where scientists can explore complex biological questions without the constraints of immediate financial return. This funding flexibility encourages the exploration of new hypotheses and unexpected findings, such as the intricate role of microglial cells in neurodegenerative diseases. As research continues to uncover the biological underpinnings of Alzheimer’s, the foundational science supported by federal funding will remain critical in developing effective treatments and improving quality of life for those affected.
Future Perspectives on Alzheimer’s Treatment
The landscape of Alzheimer’s treatment is continuously evolving, with a growing emphasis on personalized medicine and targeted therapies. Research led by scientists like Beth Stevens aims to integrate findings from cellular studies, particularly regarding microglial activity, into potential therapeutic options. Through understanding how these cells interact with neurons and their environment, there is hope for creating interventions that can slow the disease’s progression or alleviate symptoms more effectively.
Advancements in biomarker development and understanding immune responses in the brain pave the way for future therapies that could change the course of Alzheimer’s. As more research clarifies the specific roles of microglial cells and other elements of the brain’s immune system, clinicians may have access to novel treatments that directly target the mechanisms driving neurodegeneration. These developments will not only enhance the quality of care for patients but also offer new hope in the fight against Alzheimer’s and other neurodegenerative diseases.
Connecting Synaptic Pruning to Disease Mechanisms
Synaptic pruning, the process through which unnecessary synapses are eliminated, is a vital aspect of healthy brain development. However, abnormal microglial activity can lead to excessive pruning, which is implicated in neurodegenerative diseases such as Alzheimer’s. Understanding the balance of synaptic pruning is crucial, as it reflects how microglial cells can contribute to either healthy or pathological brain function. Beth Stevens’ research has shown that this imbalance plays a significant role in various neurodegenerative disorders, shedding light on potential therapeutic targets.
Exploring the connection between synaptic pruning and the onset of diseases like Alzheimer’s provides critical insights into how disruptions in normal brain function can lead to cognitive decline. By studying how microglial cells regulate this process, researchers can develop strategies to promote healthy pruning and potentially mitigate the effects of neurodegeneration. This line of inquiry not only enhances our understanding of Alzheimer’s but also informs broader approaches to treating various cognitive disorders.
Curiosity-Driven Research and Breakthroughs in Neurology
Curiosity-driven research in neuroscience is essential for fostering innovation and discovery. Scientists like Beth Stevens exemplify how pursuing fundamental questions about brain function can lead to breakthroughs with profound implications for diseases such as Alzheimer’s. This approach often leads to unexpected findings that challenge existing paradigms and open new avenues for exploration. The discoveries emerging from curiosity-driven research are what lay the groundwork for future treatments and advancements in understanding complex brain disorders.
The emphasis on fundamental research is critical in neurology, where many diseases remain poorly understood. By investing in high-risk, high-reward studies, researchers can develop innovative therapies based on new insights gained from their investigations. The work of Stevens and others highlights the importance of fostering a scientific environment that values inquiry and exploration, ultimately paving the way for transformative approaches to treating Alzheimer’s and similar neurodegenerative diseases.
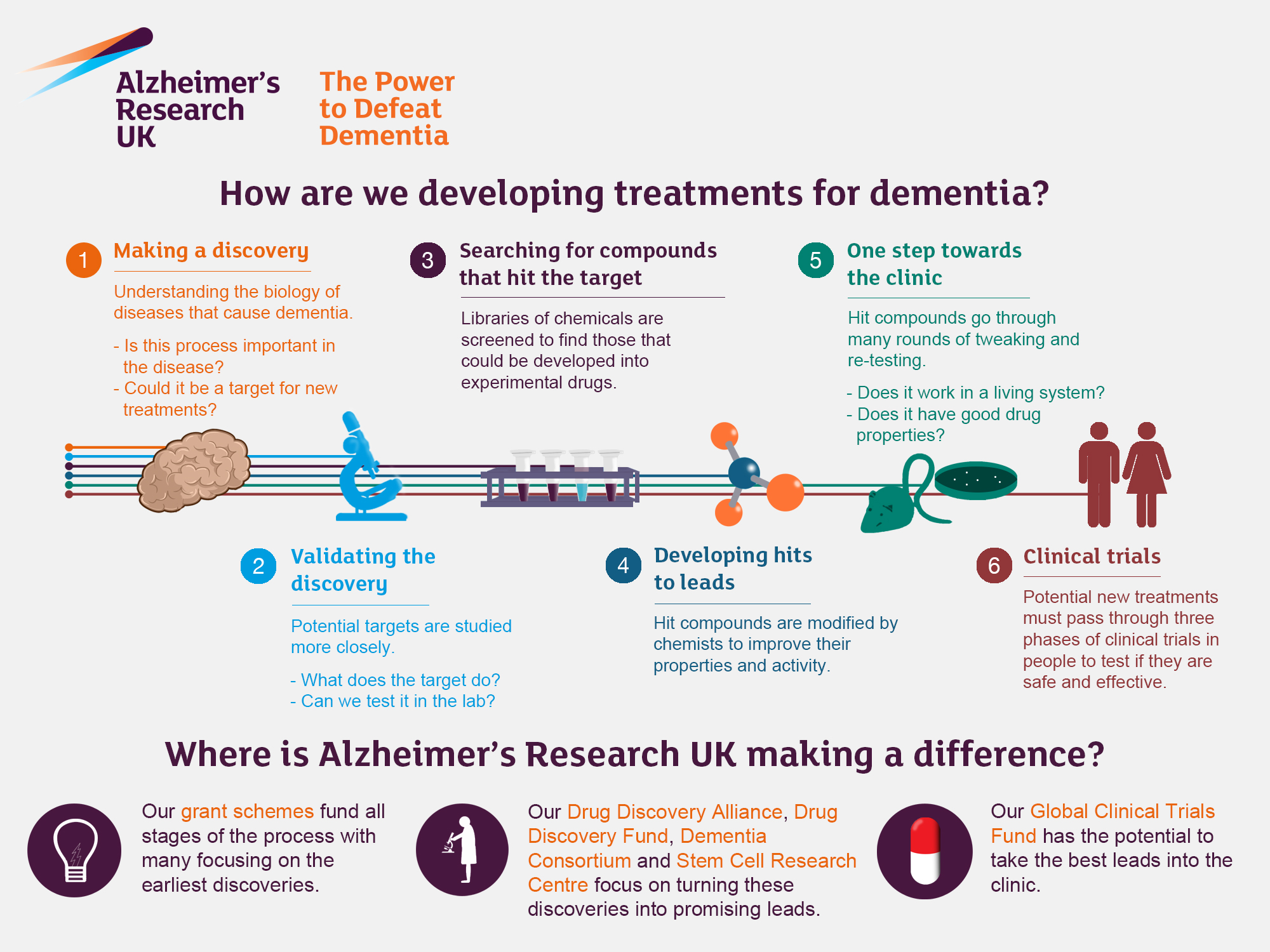
The Journey from Basic Science to Clinical Applications
The transition from basic science to clinical application is often a long and complex journey, especially in the field of Alzheimer’s research. Understanding the underlying cellular mechanisms, such as those involving microglial cells, is a critical first step that can lead to innovative clinical solutions. Beth Stevens’ work illustrates how studying foundational biological processes can result in significant advancements in understanding and treating neurodegenerative diseases. Her lab’s focus has yielded insights into how microglia can both protect and harm neural function, indicating new pathways for potential therapies.
Transforming these scientific discoveries into clinical practice requires collaboration among researchers, clinicians, and funding agencies. The support from federal entities has been instrumental in allowing scientists to explore the basic biology of Alzheimer’s and develop applicable therapies. As researchers continue to connect fundamental findings with clinical needs, the potential to enhance diagnosis and treatment for millions affected by Alzheimer’s becomes ever more attainable. Understanding this journey helps clarify the vital importance of ongoing investment in neuroscience and Alzheimer’s research.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s research?
Microglial cells are essential in Alzheimer’s research as they act as the brain’s immune system. They monitor the brain for signs of injury or illness, aiding in the removal of damaged cells and the pruning of synapses. Research by Beth Stevens has shown that abnormal microglial activity can contribute to neurodegenerative diseases, including Alzheimer’s, highlighting their importance as a target for new therapies.
How are biomarkers for Alzheimer’s disease being identified through research?
Research focused on microglial cells, such as the work done by Beth Stevens, is critical for identifying biomarkers for Alzheimer’s disease. These biomarkers help in the early detection and tracking of Alzheimer’s progression by indicating changes in brain immune responses and synaptic pruning processes, thus paving the way for potential therapeutic interventions.
What impact do neurodegenerative diseases have on microglial function?
Neurodegenerative diseases like Alzheimer’s can significantly alter microglial function. Research indicates that these alterations can lead to inappropriate pruning of synapses, which may exacerbate cognitive decline. Understanding these changes in microglial behavior is crucial for developing targeted therapies aimed at restoring normal brain function.
How has Beth Stevens contributed to the field of Alzheimer’s research?
Beth Stevens has made significant contributions to Alzheimer’s research by uncovering the role of microglial cells in brain health. Her pioneering work has revealed how these cells influence synaptic pruning, which can affect the onset and progression of Alzheimer’s disease. Stevens’ insights have opened new avenues for identifying biomarkers and developing treatments for this debilitating condition.
What is the relationship between microglial cells and the brain’s immune system in Alzheimer’s research?
In Alzheimer’s research, microglial cells are a critical component of the brain’s immune system. They protect the brain by clearing dead cells and debris, but dysregulation in their activity can lead to Alzheimer’s disease. Research by Beth Stevens emphasizes how understanding microglial function can shed light on disease mechanisms, paving the way for innovative therapeutic strategies.
Why are microglial cells considered a promising target for Alzheimer’s therapies?
Microglial cells are considered a promising target for Alzheimer’s therapies because they play a crucial role in maintaining brain health and responding to injury. Abnormalities in their function are linked to Alzheimer’s pathology. Beth Stevens’ research provides insights into how modulating microglial activity could lead to effective treatments and improve outcomes for individuals living with Alzheimer’s.
| Key Point | Details |
|---|---|
| Role of Microglial Cells | Microglia act as the brain’s immune system, responsible for cleaning up dead cells and pruning synapses. |
| Impact on Alzheimer’s Disease | Abnormal pruning by microglia is linked to Alzheimer’s and other neurodegenerative diseases. |
| Innovations in Research | Research has led to potential new biomarkers and treatments for neurodegenerative diseases. |
| Importance of Foundational Research | Sustained support from NIH and federal agencies allows for significant discoveries in Alzheimer’s research. |
| Historical Context | Beth Stevens commenced her research during the early 2000s with a focus on the immune system in the brain. |
Summary
Alzheimer’s research is crucial for addressing the challenges faced by millions suffering from this devastating disease. Recent discoveries about microglial cells have reshaped our understanding of how the brain’s immune responses affect neurodegenerative processes. By leveraging foundational research, scientists like Beth Stevens are uncovering the links between abnormal cell activity and Alzheimer’s, paving the way for innovative treatments that could improve patient outcomes. As we continue to support and invest in such vital research, we move closer to finding solutions that can transform lives.