AI pediatric cancer risk prediction is revolutionizing the way we approach the fight against childhood cancers, particularly in the context of brain tumors such as gliomas. Recent advancements in artificial intelligence have enabled researchers to accurately assess the risk of relapse in pediatric patients, thus enhancing early interventions and treatment strategies. With traditional prediction methods falling short, this innovative technology analyzes multiple brain scans over time, resulting in an accuracy rate that far surpasses conventional techniques. By employing AI in medicine, healthcare professionals can identify which children are at the greatest risk for tumor recurrence, allowing for more tailored and effective glioma treatment. The integration of temporal learning in healthcare not only improves patient outcomes but also alleviates the emotional burden associated with frequent imaging, leading to a brighter future for young cancer patients.
The concept of predicting pediatric cancer risks using advanced technology is gaining traction, particularly through the lens of artificial intelligence (AI). This innovative approach leverages historical medical data and imaging to forecast potential relapses in children diagnosed with serious conditions, such as brain tumors. By utilizing methods that allow AI to learn from repeated observations and changes over time, researchers are forging new paths in the treatment of childhood cancers. The focus on monitoring glioma recurrence illustrates how temporal learning can provide insights that enhance care for pediatric patients. As this field evolves, the use of predictive analytics in monitoring health could reshape the standards of pediatric oncology.
Advancements in AI for Pediatric Cancer Diagnosis
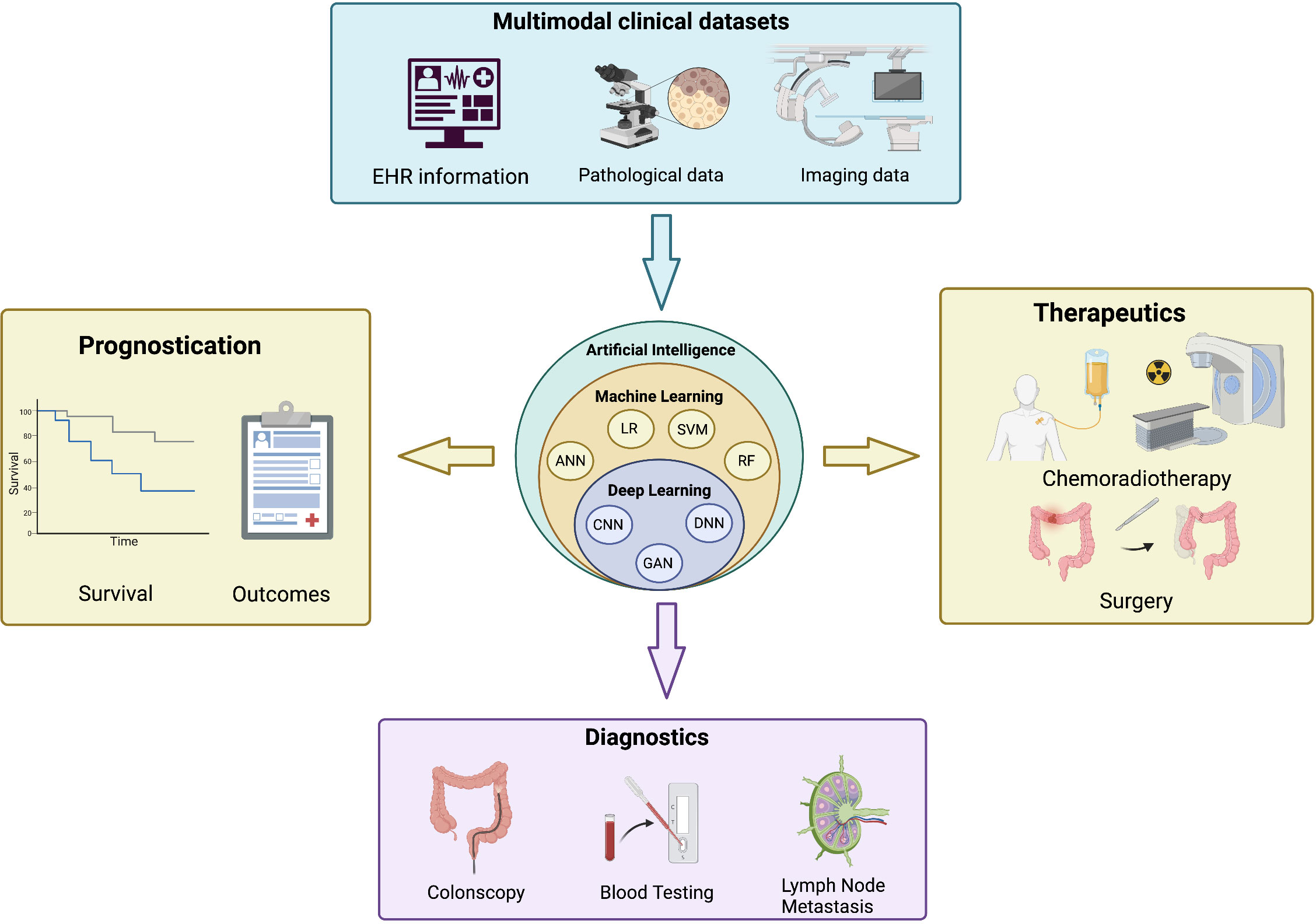
Recent advancements in artificial intelligence (AI) have paved the way for innovations in pediatric cancer diagnosis, particularly in predicting the likelihood of brain tumor recurrence. Traditional methods have often struggled to provide accurate predictions, leading to unnecessary imaging and anxiety for both patients and families. The new AI tools leverage vast amounts of data from MR scans to offer a more nuanced analysis, potentially changing the landscape of pediatric oncology. By utilizing improved algorithms, healthcare providers can now gain insights that were previously elusive, thereby enhancing diagnostic accuracy and patient management.
Moreover, this AI tool not only focuses on individual scan analysis but integrates a temporal learning approach, which reviews multiple scans taken over time. This methodology allows for a comprehensive view of a patient’s progress, essential for conditions like gliomas where recurrence risk is a concern. The integration of AI into pediatric cancer diagnosis can lead to personalized treatment plans, significantly improving outcomes for young patients facing these challenges.
The Role of Temporal Learning in Predicting Glioma Recurrences
Temporal learning represents a groundbreaking advancement in the realm of AI-based medical imaging, particularly in predicting glioma recurrences among pediatric patients. Unlike traditional models that base their predictions on isolated scans, temporal learning allows AI systems to analyze trends and detect subtle changes in brain scans collected over time. This approach has demonstrated a notable increase in accuracy, providing healthcare professionals with a powerful tool to forecast potential relapses more effectively.
Through the implementation of temporal learning, researchers have achieved impressive results, citing accuracy levels between 75-89 percent in predicting glioma recurrence within one year post-treatment. This decreased reliance on singular images sharpens the model’s predictive capabilities, which is crucial for optimizing follow-up strategies for pediatric cancer patients. As the clinical landscape evolves, the integration of temporal learning may redefine standard practices in pediatric oncology and enhance how healthcare providers approach glioma treatment.
AI Pediatric Cancer Risk Prediction: A Revolutionary Approach
The introduction of AI pediatric cancer risk prediction tools marks a revolutionary shift in the management of pediatric oncology. By processing and analyzing thousands of MRI scans, these AI systems provide a level of predictive accuracy that surpasses traditional methodologies. This new approach not only identifies patients at high risk of recurrence but also streamlines the follow-up process, reducing both psychological and logistical burdens on families. With an improved understanding of which children may benefit from closer monitoring, oncologists can make more informed decisions about treatments and interventions.
Furthermore, the potential for AI-informed risk assessments to trigger targeted therapies for high-risk patients is particularly promising. As more data becomes available and models become fine-tuned, the ramifications for treatment protocols could be profound. Improved risk prediction is not just about enhancing individual patient care; it represents a broader commitment to leverage cutting-edge technologies to elevate the standards of pediatric cancer treatment and long-term survival outcomes.
Impact of AI on Treatment Strategies for Pediatric Gliomas
AI technologies are revolutionizing treatment strategies for pediatric gliomas, enabling a more individualized approach based on precise predictions of tumor recurrence. This advancement allows oncologists to utilize data-driven insights when designing treatment plans, ensuring that interventions are both timely and effective. AI’s capacity to predict relapses can help medical teams decide when to initiate additional therapies or adjust treatment protocols, potentially improving overall patient outcomes and reducing unnecessary treatments.
Moreover, by providing accurate assessments of recurrence risk, AI can significantly impact the frequency and timing of follow-up imaging. Tailoring follow-up schedules based on individual recurrence probabilities enhances the patient experience and alleviates the strain on healthcare resources. The shift towards AI-integrated treatment pathways signifies a concerted effort to blend technology with medicine, ensuring that children diagnosed with gliomas receive the best possible care.
Ethical Implications of AI in Pediatric Oncology
As AI continues to make inroads into pediatric oncology, it brings forth significant ethical considerations that must be addressed. The accuracy of AI-based tools in predicting cancer recurrence raises questions about the implications of false positives or negatives in prognosis. Ensuring that AI predictions align with ethical standards in healthcare is paramount, as decisions based on these tools can dramatically affect a child’s treatment journey and their families’ emotional well-being.
Furthermore, the development and implementation of AI systems require transparent communication with patients and caregivers about how their imaging data is utilized. Emphasizing the secure and ethical management of sensitive health information is critical, fostering trust in AI systems amongst stakeholders. Establishing a framework to address these ethical challenges will be essential as AI becomes increasingly integral in shaping the future of pediatric cancer care.
Clinical Trials: The Next Steps for AI Prediction Tools
Following promising results from studies utilizing AI in predicting pediatric cancer recurrence, the next logical step involves conducting clinical trials to validate these findings in real-world scenarios. These trials will be crucial to determine the efficacy and reliability of AI tools in diverse clinical settings, ultimately shaping guidelines for their use in pediatric oncology. Armed with data from clinical environments, researchers can refine AI models, ensuring they meet the varying needs of patients under different treatment regimes.
Moreover, clinical trials will assess the potential of AI-informed risk predictions to alter current practices regarding imaging frequency and treatment interventions. By demonstrating tangible benefits in patient outcomes and resource utilization, these trials could lead to widespread acceptance and integration of AI technologies across healthcare systems. The successful implementation of AI risk prediction tools can catalyze a new era in pediatric oncology, marked by precision, personalization, and improved survival rates.
Challenges in Integrating AI into Pediatric Healthcare
While the promise of AI in pediatric oncology is significant, integrating these advanced technologies into existing healthcare infrastructures presents multiple challenges. One of the foremost hurdles is ensuring that clinicians are adequately trained to interpret and act on AI-generated predictions. As these tools become a crucial part of clinical decision-making, healthcare professionals must develop confidence in using AI insights alongside traditional methods, fostering a collaborative landscape where technology augments professional expertise.
Additionally, the reliance on large datasets to train AI algorithms raises concerns about data quality and representation. Ensuring that AI models are trained on diverse populations is essential to prevent bias in predictions, particularly when it comes to conditions like pediatric cancer, where variations exist in tumor biology and treatment responses. Overcoming these barriers will be essential to harnessing the full potential of AI in transforming pediatric cancer care.
The Future of AI in Medicine: Pediatric Cancer Focus
The future of AI in medicine, particularly within pediatric oncology, is filled with potential as new developments continue to emerge. As researchers explore innovative techniques such as temporal learning and advanced imaging processing, the accuracy of AI-based predictions will only improve. This advancement could eventually lead to AI systems being standard tools in clinics, guiding treatment decisions and optimizing care pathways for children diagnosed with cancer.
Moreover, as we witness rapid technological advancements, the collaboration between clinical practitioners and data scientists will be critical in shaping the effective use of AI in medicine. By focusing on real-world applications and outcomes, the integration of AI tools can greatly benefit pediatric oncology. As successful models arise, the future landscape will see a blend of cutting-edge approaches that not only enhance patient care but also hold promise for better understanding and treating various forms of pediatric cancer.
Frequently Asked Questions
How does AI pediatric cancer risk prediction improve the accuracy of brain tumor recurrence forecasts?
AI pediatric cancer risk prediction utilizes advanced algorithms and temporal learning techniques to analyze multiple brain scans over time, dramatically improving the accuracy of brain tumor recurrence forecasts. This approach allows for the identification of subtle changes across scans that indicate potential relapse, achieving prediction accuracies between 75-89%, compared to traditional methods that typically only reach approximately 50% accuracy.
What role does temporal learning play in AI pediatric cancer risk prediction?
Temporal learning is a critical component of AI pediatric cancer risk prediction, as it enables the analysis of sequential brain imaging data. By incorporating changes observed in multiple scans taken over time, the AI model enhances its ability to detect patterns that correlate with cancer recurrence, leading to earlier and more accurate predictions for pediatric patients with gliomas.
Can AI in medicine really change how we manage pediatric cancer patients?
Yes, AI in medicine, especially through pediatric cancer risk prediction, has the potential to transform management approaches by providing more precise assessments of relapse risk. This can lead to tailored treatment plans that optimize care, reduce unnecessary imaging procedures for low-risk patients, and enable proactive interventions for those at higher risk of recurrence.
How effective are AI tools at predicting pediatric glioma recurrence compared to traditional methods?
AI tools designed for pediatric cancer risk prediction have shown significantly higher effectiveness in predicting glioma recurrence. With an accuracy range of 75-89% through the use of temporal learning and analysis of multiple scans, these tools outpace traditional methods that rely on single images, which provide only about 50% accuracy.
What implications do AI-driven predictions have for the treatment of pediatric brain tumors?
AI-driven predictions in pediatric cancer risk assessment can lead to personalized treatment plans, whereby low-risk patients may benefit from reduced imaging and monitoring stress, while high-risk patients could receive timely and tailored therapies, potentially improving overall outcomes in glioma treatment.
What kind of data is analyzed for AI pediatric cancer risk prediction?
AI pediatric cancer risk prediction analyzes longitudinal data from multiple magnetic resonance imaging (MRI) scans collected over time. By evaluating these scans, researchers can detect changes that indicate the likelihood of tumor recurrence, thus enhancing the predictive power of AI models in managing pediatric cancer.
Are there any clinical trials planned to test AI in pediatric cancer risk prediction?
Yes, researchers are planning to initiate clinical trials aimed at validating AI-informed risk predictions in pediatric cancer care. These trials will assess whether the integration of AI can effectively enhance patient management, ensuring both safety and improved outcomes for high-risk pediatric glioma patients.
| Key Points |
|---|
| AI tool shows improved accuracy in predicting pediatric cancer relapse risk compared to traditional methods. |
| Research focused on pediatric gliomas, which can be treated with surgery but may have unpredictable relapse risks. |
| Temporal learning technique analyzes multiple brain scans over time to enhance prediction accuracy. |
| Study conducted on nearly 4,000 MR scans from 715 pediatric patients, showing a prediction accuracy of 75-89%. |
| The findings may lead to improved clinical practices, including fewer follow-ups or targeted therapies for high-risk patients. |
Summary
AI pediatric cancer risk prediction has emerged as a groundbreaking development in managing pediatric gliomas. By employing advanced techniques such as temporal learning, researchers have significantly enhanced the accuracy of relapse risk predictions. This innovative approach not only reduces the anxiety and burden on families but also paves the way for a more tailored treatment strategy. With prediction rates soaring to 75-89%, clinical trials are poised to explore the full potential of AI in safeguarding the future of pediatric oncology.