Brain cancer prediction in children is a critical area of research that has recently seen advancements thanks to innovative AI technologies. A groundbreaking study from Mass General Brigham highlights how an artificial intelligence tool has significantly improved the accuracy of predicting relapse risks in pediatric gliomas compared to traditional methods. By analyzing thousands of MRI scans over time, researchers were able to harness the power of temporal learning AI to detect subtle changes in patients’ conditions, paving the way for more effective monitoring and treatment. This promising approach not only eases the burden of frequent imaging for families but also opens up pathways for personalized interventions in predicting cancer relapse. Ultimately, the goal is to enhance care for young patients battling brain tumors, transforming how we approach pediatric cancer treatment and outcomes for the future.
In the realm of childhood cancer, particularly concerning brain tumors, the ability to foresee potential recurrences has become increasingly important. Recent developments in artificial intelligence have led to new methodologies for assessing pediatric glioma relapse risk, enhancing MRI scans for pediatric cancer patients. Researchers are exploring unique predictions through advanced machine learning techniques that analyze multiple imaging sessions over time instead of relying on singular scans. By leveraging temporal learning AI, the hope is to provide a more nuanced understanding of a child’s condition, ultimately making strides in predicting cancer relapse and tailoring treatments accordingly. This innovative approach signifies a major shift in pediatric oncology practices, striving to safeguard the health and future of young cancer patients.
The Role of AI in Predicting Pediatric Glioma Recurrence
Artificial Intelligence (AI) is transforming how we predict brain cancer relapse in children, particularly in pediatric glioma cases. Traditional methods often fell short in accurately assessing a patient’s risk for recurrence, relying largely on single MRI scans and subjective interpretations. However, the integration of AI in cancer treatment, especially with tools analyzing multiple MRI scans over time, marks a significant advancement. By employing temporal learning algorithms, researchers can not only detect subtle changes in brain scans but also enhance prediction accuracy, giving families better insights into their child’s health post-treatment.
In a recent study conducted by Mass General Brigham, researchers demonstrated that their AI tool could predict the risk of cancer relapse up to 89% accurately, compared to merely 50% using conventional methods. This leap in predictive capability highlights the urgency of incorporating AI technology into pediatric oncology. Not only does it promise more personalized care plans, but it also reduces the emotional toll on both patients and families frequently subjected to anxiety-ridden follow-up scans. As the landscape of pediatric cancer care evolves with innovative solutions, the focus remains on developing AI models that can safely and effectively guide treatment decisions.
MRI Scans: Vital Tool in Pediatric Cancer Care
Magnetic Resonance Imaging (MRI) scans play a crucial role in the management and monitoring of pediatric cancers. Frequent imaging is necessary for detecting any potential relapses, particularly in brain tumors such as gliomas that are treated through surgery. The challenge, however, lies in the discomfort and anxiety these repeated procedures can cause for young patients. AI advancements, specifically temporal learning models, seek to mitigate this burden by optimizing how we interpret MRI data, leading to more efficient surveillance protocols.
The implications of AI-enhanced MRI analysis extend beyond just improved accuracy. Pediatric cancer patients may benefit from a reduced frequency of imaging, allowing for a more comfortable experience. As AI continues to perfect its predictive capabilities, healthcare providers aim to identify those patients most at risk of recurrence, which can guide clinical efforts and ensure that appropriate interventions are made promptly. This shift promises to mark a new era in pediatric oncology where caregivers can allocate resources more effectively and enhance the quality of life for their young patients.
Temporal Learning in Cancer Predictions
Temporal learning represents a groundbreaking approach in the realm of cancer prediction, especially as it pertains to childhood brain tumors. Unlike traditional models that might only evaluate a single moment captured in an MRI scan, temporal learning uses a sequence of images taken during a patient’s recovery phase. This method allows AI to recognize patterns and changes over time that might indicate the early signs of glioma recurrence. By synthesizing past data, the AI can create a comprehensive view of each patient’s status, improving the chances of catching potential problems early.
The study findings that showcase predictive accuracy ranging from 75% to 89% underscore the value of employing this novel methodology. By increasing the number of MRI scans analyzed, researchers were able to enhance their model’s performance, pinpointing when a patient’s condition may begin to deteriorate. This dynamic approach pivots away from static diagnostic methods, highlighting the necessity for continuous monitoring integrated with advanced AI analytics. Ultimately, temporal learning opens new frontiers for predicting not just glioma recurrence but potentially redefining approaches to monitoring other pediatric cancers as well.
Improving Pediatric Cancer Treatment with AI
AI’s incorporation into pediatric cancer treatment heralds a new phase in personalized medicine. Recognizing that early detection of recurrence can significantly alter treatment outcomes, researchers are enthusiastic about the application of AI in analyzing complex datasets from multiple MRI scans. This technology aims to empower healthcare providers with more precise predictions regarding which patients might need more vigilant monitoring versus those who may benefit from a less aggressive follow-up schedule.
Additionally, AI’s potential to assist in treatment planning is being explored. By more accurately forecasting which children are at higher risk for glioma recurrence, practitioners can employ targeted therapies tailored to individual conditions. This not only optimizes the care pathway for patients but also opens the door for enhanced clinical trials. Employing AI-informed insights could lead to further breakthroughs in pediatric oncology as innovation continues to shape the future of healthcare.
The Future of Pediatric Oncology and AI Integration
The future of pediatric oncology is becoming increasingly intertwined with artificial intelligence, promising significant advancements in care and outcomes. As AI technology becomes more advanced, treatments tailored specifically to the unique needs of children with brain cancers like gliomas will become more prevalent. Innovative predictive models will not only assist in early detection of recurrences but may also inform decisions surrounding preventative measures that could improve overall survival rates.
Moreover, the collaborative efforts between medical institutions, such as the partnerships seen in Harvard’s recent studies, validate the strength of integrating AI into healthcare. By pooling resources and data, researchers can enhance their models, ensuring that predictions are as accurate and actionable as possible. As the development of these technologies continues, the hope is that pediatric patients will experience better tailored therapies, reduce the frequency of invasive procedures, and above all, enhance their quality of life during and after treatment.
Potential Challenges in AI Application for Cancer
While the prospects for AI in predicting pediatric cancer recurrence are promising, significant challenges remain. One of the primary concerns is the need for extensive validation of AI models in diverse clinical settings. The performance of these algorithms can vary depending on the patient population and the imaging techniques employed. Ensuring their reliability before they are applied broadly in clinical practice requires further studies and refinements.
Additionally, disparities in access to advanced AI technologies among different healthcare facilities could pose barriers. There is a risk that not all patients will benefit equally from these innovations, potentially widening existing gaps in healthcare equity. Addressing these issues is crucial as stakeholders push for the integration of AI into standard pediatric oncology practice, ensuring that advances translate into equitable care for all children facing brain cancer.
The Importance of Continuous Research in Pediatric Cancer Treatments
Continuous research is vital in advancing the understanding and treatment of pediatric cancers, particularly brain tumors. As studies unveil new methodologies and tools, like AI-driven predictive models, they set the stage for more effective clinical practices. Ongoing exploration into the underlying biology of pediatric gliomas combined with technological innovation ensures that our approaches remain effective and responsive to the needs of young patients.
Furthermore, the collaboration among healthcare providers, researchers, and tech innovators fosters an ecosystem where the latest findings can rapidly translate into practice. This continuous loop of feedback and refinement will likely lead to breakthroughs that not only improve prediction accuracy but also enhance treatment protocols. As we forge ahead in leveraging AI and advanced imaging techniques, the collective aim remains to provide the best outcomes possible for children battling cancer.
Training and Education on AI and Pediatric Oncology
As AI technologies become increasingly pivotal in pediatric oncology, the need for comprehensive training and education for healthcare providers is evident. Understanding how to effectively utilize these tools, interpret AI-generated data, and integrate findings into treatment planning requires specialized knowledge. Institutions must prioritize educational initiatives that will equip oncologists, nurses, and radiologists with the skills necessary to harness AI’s capabilities fully.
Moreover, educating families about how AI impacts their child’s care can foster better communication and understanding. Patients and their guardians should be informed about what AI can predict and how these predictions can influence treatment decisions. This transparency is essential in building trust and ensuring that all stakeholders are aligned in the approach toward pediatric cancer care.
The Global Impact of AI on Pediatric Healthcare
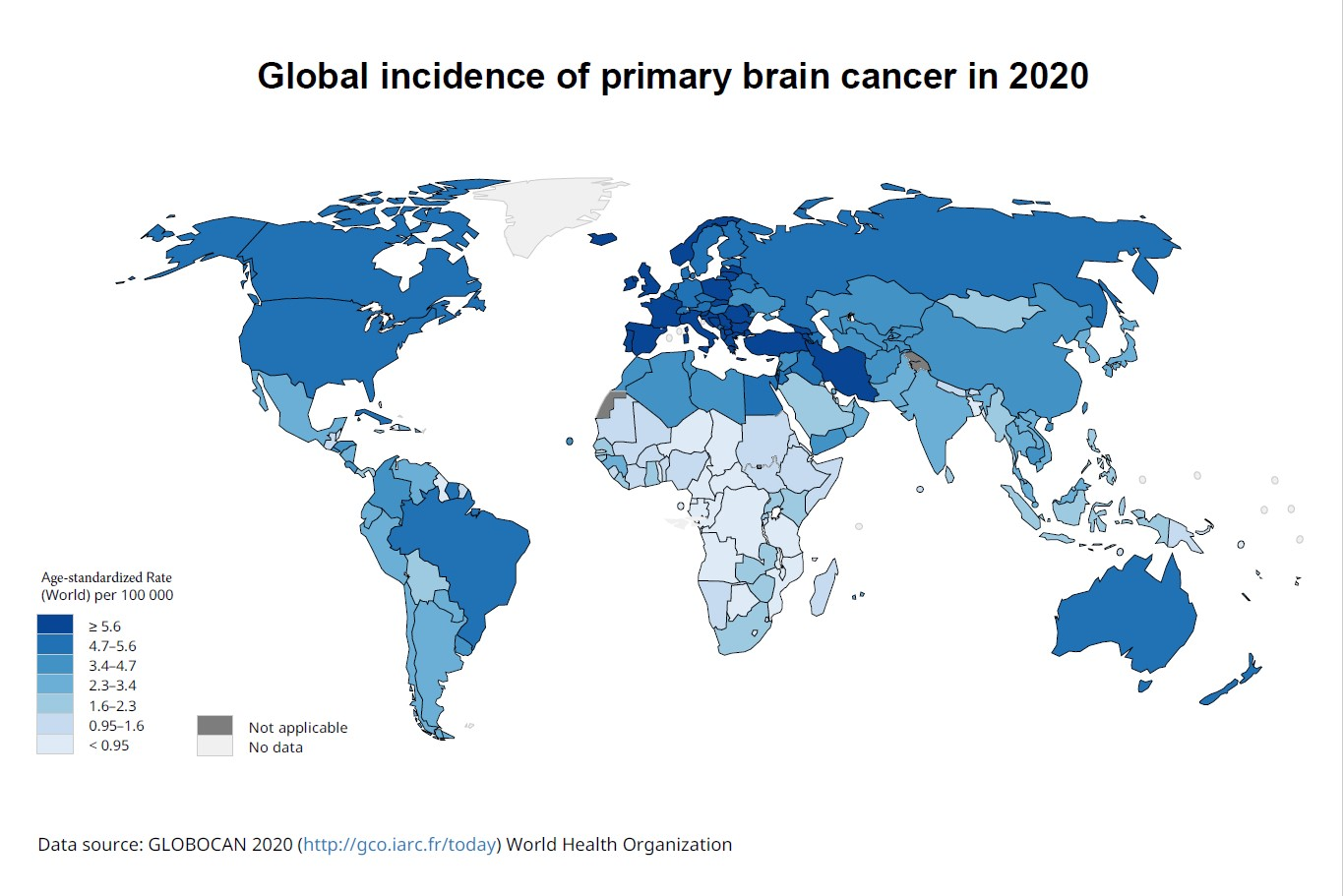
Expanding the conversation beyond local hospitals, the global implications of AI integration in pediatric healthcare are profound. Through international collaborations and data sharing, researchers can create more robust AI models that account for diverse populations and healthcare contexts. This not only enhances the accuracy of predictions for pediatric glioma recurrences but also promotes best practices across borders.
As AI tools spread worldwide, they could revolutionize the way pediatric cancers are treated on a global scale. Low-resource settings stand to gain significantly from AI’s efficiency, optimizing limited healthcare resources while improving patient outcomes. The vision for a future with enhanced pediatric cancer care is indeed a global effort, relying on innovative technologies that transcend geographic boundaries and improve lives everywhere.
Frequently Asked Questions
How does AI enhance brain cancer prediction in children?
AI enhances brain cancer prediction in children by analyzing multiple MRI scans over time, utilizing techniques such as temporal learning. This approach allows AI tools to identify subtle changes that may indicate the risk of recurrence in pediatric glioma patients, significantly improving prediction accuracy over traditional single-scan techniques.
What is temporal learning in AI for pediatric brain cancer?
Temporal learning in AI for pediatric brain cancer involves training algorithms to analyze a series of MRI scans taken over time, rather than relying on individual images. This method helps the AI detect progressive changes in the brain, leading to more accurate predictions of cancer relapse in children with conditions like gliomas.
What role do MRI scans play in predicting brain cancer relapse in children?
MRI scans are crucial for predicting brain cancer relapse in children, as they provide detailed images of brain tumors. Recent studies have shown that using multiple MRI scans along with AI tools can significantly increase the prediction accuracy of relapse in pediatric patients, especially those with gliomas.
Can AI tools predict pediatric glioma recurrence?
Yes, AI tools can predict pediatric glioma recurrence with greater accuracy than traditional methods. A study indicated that AI models utilizing temporal learning could achieve an accuracy rate of 75-89% in predicting relapse within one year post-treatment, based on an analysis of serial MRI scans.
How effective are traditional methods for brain cancer prediction in children?
Traditional methods for brain cancer prediction in children have a prediction accuracy of around 50%, which is comparable to random chance. This highlights the need for advanced techniques like AI and temporal learning, which can analyze multiple scans to provide much more reliable predictions.
What advancements are being made in AI for pediatric cancer treatment?
Advancements in AI for pediatric cancer treatment include the development of models that use temporal learning to analyze changes in MRI scans over time. These innovations are expected to improve the accuracy of predicting relapse in pediatric glioma patients and could ultimately enhance treatment plans and patient care.
Why is predicting cancer relapse important for children’s health?
Predicting cancer relapse is crucial for children’s health because early identification of high-risk patients can lead to tailored treatment plans, potentially reducing the frequency of stressful follow-up imaging procedures and enabling timely interventions for effective management of pediatric brain tumors.
What are the implications of improved AI prediction models for pediatric gliomas?
Improved AI prediction models for pediatric gliomas could allow for personalized treatment approaches, where low-risk patients might experience fewer MRIs, while high-risk patients could receive pre-emptive targeted therapies. This shift has the potential to enhance overall care quality and patient outcomes in children with brain cancer.
| Point | Details |
|---|---|
| Research Focus | Catching brain cancer relapse in children using AI predictive tools. |
| AI Tool | An AI tool surpasses traditional methods in predicting relapse risk for pediatric gliomas. |
| Study Institutions | Conducted by Mass General Brigham, Boston Children’s Hospital, and Dana-Farber Cancer Center. |
| Temporal Learning | Utilizes data from multiple MRI scans over time to improve prediction accuracy. |
| Prediction Accuracy | Accuracy of 75-89% for predicting recurrence, significantly better than 50% with single images. |
| Future Plans | The goal is to conduct clinical trials to validate AI predictions in improving patient care. |
| Implications | Potential to personalize treatment plans and reduce unnecessary follow-up imaging. |
Summary
Brain cancer prediction in children has seen significant advancements thanks to the introduction of AI tools developed in recent studies. These tools not only improve the accuracy of predicting relapse in pediatric glioma patients but also aim to enhance care practices, potentially leading to better outcomes and reduced stress for families. As the research progresses, the integration of AI into clinical settings may revolutionize how pediatric brain cancer is monitored and treated.